To operate or not to operate was the question addressed at the tonsillectomy and adnoidectomy (T. and A.) section of the Dartmouth-Hitchcock Medical Center conference on pediatric otolaryngology in May. In the days before antibiotics, the operation was routine for young children, and those of us past 30 are predictably tonsil-bereft. The tonsil and adenoid masses in the back of the throat (which may have some immunologic value, though nobody knows for sure) were supposed to harbor infectious bacteria, and one or both were surgically removed when children were four, five, or six in order to prevent strep throat, a common childhood illness that can lead to heart-impairing rheumatic fever. The operation was also thought to cure recurrent otitis media, or inflammation of the middle ear, another common ailment of children under seven.
After strep throat succumbed to antibiotics, the incidence of T. and A. dropped, though not as much as many doctors felt it should have done, given the risks of general anesthesia and post-operative bleeding and the lack of evidence linking middle ear disease with tonsils and adenoids. During the seventies, a push was made to break the back of the habitual performance of T. and A.s by pediatricians. The result was that T. and A. dropped from top place as the most frequent operation in the country in 1972 to fifth place in 1979 (though it remains the most frequent of all operations for males).
Now, according to conference organizer Dudley Weider of the Dartmouth-Hitchcock faculty, the pendulum has swung too far; and a major medical controversy has erupted over what circumstances, if any, warrant tonsillectomy, adenoidectomy, or both. The research described at the conference focused on the obligate mouthbreather, the child whose upper airway is severely or totally blocked by tonsil or adenoid mass.
Among the featured speakers were Charles Bluestone, professor of otolaryngology at the University of Pittsburgh Medical School (where a large study of T. and A. is underway), and Jerome Klein, professor of pediatrics at the Boston University School of Medicine and director of a large infectious diseases unit at Boston City Hospital. Bluestone discussed techniques of measuring mouth-breathing in young children whose nasal obstruction is neither allergic nor the result of sinusitis. Parents tape-record the sounds a mouthbreathing child makes two hours into the night's sleep for evidence of snoring and episodes of sleep apnea (disturbance) resulting from unsuccessful efforts to breathe smoothly. If sleep patterns and speech distortion warrant it, a neck x-ray is also taken, which will often show clearly how the upper airway is blocked. As part of the Pittsburg study, children are also sometimes "wired up" in sleep labs for detailed information on their oxygen intake patterns. One unexpected result of this latter procedure has been evidence of a connection between enuresis (bed-wetting) and nasal obstruction.
Epidemiologist Klein offered statistical evidence of the confused state of T. and A. practice, citing an "extraordinary" geographical variation in incidence of the operation. He called for bush-beating efforts to involve local physicians in T. and A. research, claiming that the focus of that research has for too long been exclusively the urban medical center. Vermont orthodontist Donald Neely supported the claim that adenoidectomy is warranted in cases of severe obstruction by discussing experiments with monkeys whose nasal passages were blocked by researchers for long periods. There is justifiable concern, he said, over the connection between mouth-breathing and poor facial growth, buck teeth, crossbite, and upper jaw collapse.
"We set up the conference to try to agree on the criteria for tonsil and adenoid surgery," said Weider, who felt when it was over that the 70 participants had, in fact, been able to agree on at least one situation that surgery would help that of certain mouth-breathing children. Otherwise, a commonsense approach involving less surgery than in the past seems to be the order of the day.
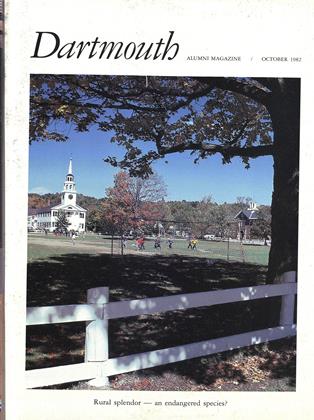 View Full Issue
View Full Issue
More From This Issue
-
 Feature
FeatureWHY STUDY WOMEN?
October 1982 By Mary Ellen Donovan -
 Feature
FeatureHome, Home on the Plain
October 1982 By Jeffrey Boffa -
 Feature
FeatureCan the Summer?
October 1982 By Shelby Grantham -
 Sports
SportsAn Irish Connection and a Quaker Shutout
October 1982 By Brad Hills '65 -
 Class Notes
Class Notes1982
October 1982 By John King -
 Article
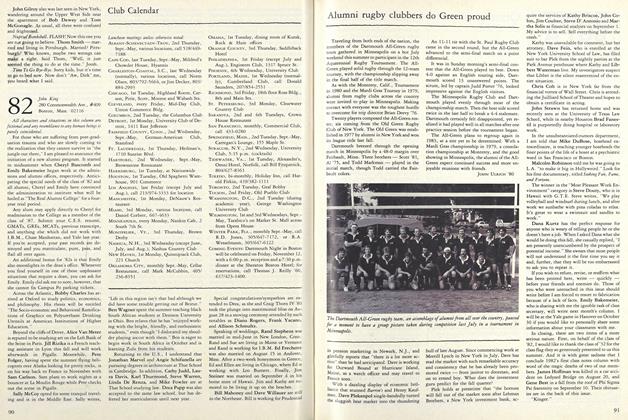
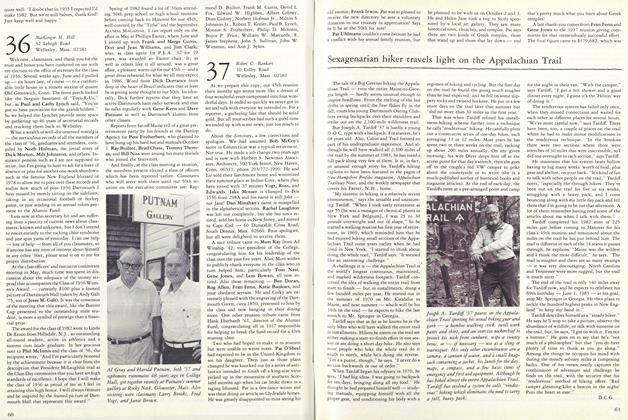
ArticleSexagenarian Hiker Travels Light on the Appalachian Trail
October 1982 By D.C.G