This age-old scourge afflicts half of all Americans. A Medical School team explores causes and cures.
MRS. Martha Groscorps - age, 28; height, 65 inches; weight, 296 pounds - was admitted to Mary Hitchcock Hospital in Hanover on an October afternoon in 1973. Acute medical emergency, no; chronic illness, unquestionably.
The diagnosis was obvious. Mrs. Groscorps was suffering from obesity, a disease which afflicts - to a greater or lesser degree - probably more than half of American adults, with all the attendant hazards of heart disease, hypertension, gall-bladder problems, diabetes, a number of other metabolic disorders, and a life span significantly shorter than normal.
Like a good proportion of grossly overweight Americans, Mrs. Groscorps had been a fat baby, cute and cuddly, with rosy dimpled cheeks, plump hands, barely discernible wrists and ankles, pudgy arms and legs with deep creases. A joy to her doting parents, she finished her bottle promptly, accepted solid foods as soon and as often as they were presented, and to the pride of mother and father, doubled and tripled her birth weight faster than any kid on the block. She had grown into a fairly lethargic teen-ager with a voracious appetite for sweets and high-calorie snacks, a preference for television over sports, and a restricted social life. At 28, married with no children, she took little interest in community activities and was virtually unemployable because of her size. She was a diabetic, and her response to insulin was poor. Honestly wanting to lose weight, she had experimented quixotically with a number of popular diets, generally abandoned after a brief time, and had sought medical help, only to be told to eat less and get some exercise, especially in the realm of self-discipline.
Desperate, Mrs. Groscorps had responded some months earlier to an extraordinary call for volunteers, issued by Dr. Lester B. Salans, associate professor of medicine at the Dartmouth Medical School, through radio and television stations and newspapers in the Hanover area. The prerequisites were only that the volunteers be obese to a significant degree and that they agree to spend several months as in-patients at the hospital, where they would be helped to control their weight and in turn would make an important contribution to the understanding of a severe and widespread public health problem.
It would be April before Mrs. Groscorps was discharged, lighter by 108 pounds; wiser, it was to be hoped; strangely apprehensive about her future. Unfortunately, the chances were better than even that before the year was out, her weight loss would be restored.
When she checked out of the hospital, she by-passed the cashier's office. Thanks to soaring hospital costs, she had accrued some $15,000 in medical bills, but she owed nothing.
ALTHOUGH Mrs. Groscorps does not exist as an individual, she serves here as a composite of some 100 volunteers who, since 1969, have participated in Dr. Salans' research program in the nature of obesity and a prototype, writ large, of millions of other Americans who face health risks and social and economic privation because of what is technically "the presence of excessive amounts of adipose tissues."
"There is no question," says Salans, "that obesity is a major public health problem or that it's received only haphazard, unsystematic, non-scientific attention from the medical profession. In the past, we have really known nothing about the disease of obesity, so we haven't been able to help much, a frustrating situation for both patient and physician."
"Obesity is not only a serious health problem, but a common one and increasingly so, a fact that has only within the last few years led to an emphasis on the need for basic research into the nature of the disease," according to Salans.
He draws a distinction between overweight and obese. An athlete in top condition is probably overweight for his or her age and height, but the excess weight is in heavy muscle tissue rather than fat deposits; a pregnant woman is obviously overweight temporarily, according to the standard tables, though optimally not obese; on the other hand, a sedentary man or woman may even be of normal weight and obese at the same time, with too large a proportion of body weight in fatty tissue.
Basic research into the causes of obesity, the chemistry of adipose tissue cells, has been the subject of investigation by Salans, a specialist in endocrinology and metabolism, since he received his M.D. in 1961 from the University of Illinois. After a residency at Stanford, he stayed on as a post-doctoral fellow in endocrinology and metabolism, with the support of the U.S. Public Health Service. Subsequently he held fellowships under similar sponsorship at Rockefeller University, where he became associate physician and assistant professor in 1967. The following year he joined the staff of the Dartmouth Medical School, where he has been director of the Section of Endocrinology and Metabolism since 1971.
In 1972 Salans received a "research career development award" from the Public Health Service and a three-year, $247,836 grant from the National Institutes of Health to support his research and the clinical program involving the Upper Valley area volunteers. He has recently received a new five-year grant of $570,000 to carry on his work.
While many laboratories across the country are conducting obesity research, Salans says, "our interest here is in better definition of the disease and how it is related to diabetes. We know that obesity is not a single entity, but a complex syndrome. Though in some rare instances we can identify a specific cause, in the overwhelming majority of cases we are still trying to determine the nature and cause of the disorder. And while we know that obesity can bring on diabetes in the diabetically prone - 90 per cent of diabetics are obese and that the chemistry of adipose tissue cells makes the obese patient's diabetes more difficult to control, we are still trying to learn how and why this happens."
So far, the most significant result of the research of Salans and his colleagues is the discovery that there are at least two distinct kinds of obesity: one hypercellular, involving a greater number of cells in the adipose tissue; the other hypertrophic, in which the cells are of normal number but grossly enlarged. "Hypercellular obesity appears to be irreversible," he says, "an Observation paralleled by the actual clinical situation, in which it is much harder to effect - and maintain - weight loss in patients found to have the hypercellular form than in those who have a normal number of cells. Furthermore, the data suggest that it is early developing obesity, particularly during infancy and about the time of puberty, which results in increased numbers of cells."
It is apparently an inherent characteristic of adipose tissue that the cells multiply during those particular periods in life, Salans explains, just as, for instance, all brain cells are formed before birth, while liver cells continue to develop as long as the organ is nourished. Thus brain cells destroyed or damaged can never be replaced, but the liver has the capacity for regeneration. Apparently, once the fatty cells have multiplied, their number is irreducible. If the individual acquires an excess of fatty tissue cells, he seems to be stuck with them for life.*
One direction of Salans' research project is to learn how, and furthermore why, adipose tissue cells tend to multiply during 'he specific limited periods of infancy and puberty. But the practical application of this investigation is a new concentration on sound nutritional education for parents and potential parents. The most intractable form of obesity, hypercellular, with all its consequent health risks, can perhaps be prevented before it occurs - by exploding the myth that "a fat baby is a healthy baby" and reducing the highcalorie
snacks, sugar-laden cereals, sweets, and soft drinks in teen-age diets more influenced by TV pitchmen than by experts in nutrition.
Fundamentally, obesity is caused by the consumption of more calories than the body expends, with the excess being stored in fatty tissue. "What hasn't been determined," Salans says, "is why some people regulate their consumption perfectly - and automatically - to fit the body's needs, and others don't." What causes abnormal appetite; why the delicate mechanism that regulates weight goes awry; whether the source of the problem is metabolic, psychological, hormonal, neurological, genetic, cultural, or a combination thereof, are among the unanswered questions.
Although some cultures past and present may smile on obesity as a symbol of plenty and well-being, being fat in America is no joke. American society, whose affluence has contributed to the alarming incidence of obesity by putting the nation on wheels instead of afoot and permitting the easy purchase of expensive "junk foods," perversely stigmatizes obesity. The old saw notwithstanding, everybody does not love a fat man - or woman. To the contrary, the obese suffer from unwarranted implications of gluttony and lack of will power, diminished job opportunities, and a certain amount of social ostracism which may intensify their problem.
"I know of no more highly motivated group than the volunteers in our program," Salans contends. "They have to want desperately to get thin to put themselves through the ordeal." Although the patients are fully apprised of the regimen before they enter the hospital, they are still discouraged, he reports, by being actually forbidden to lose weight for
the first two months of their stay. During that time, they are kept strictly on their normal diets of probably 3,000 calories. Meanwhile, they undergo intensive testing to ascertain how their bodies use the calories they consume, how their adipose tissue cells react to the foods they normally eat; if they are diabetic, whether: they have become diabetic because they were fat or fat because they were diabetic; whether they have hypercellular obesity or a normal number of cells grown very large. Samples of their tissues are studied to see how they perform in test tubes, watched to see how the cells make fat, how they respond to different kinds of calories.
As the program progresses and the patients' diets are reduced to à 600-calorie weight-loss regimen, the testing goes on, to observe how their metabolism changes as the cell size is reduced, to study the effect of different diets. Simultaneously, a routine of carefully supervised exercise primarily walking and swimming in the College pool - is introduced.
At one time, a program of behavioral modification was instituted, under the direction of a clinical psychologist from the Department of Psychiatry, to help the patients break old patterns of consumption and re-orient their habits, associations, and attitudes toward food. Budget cuts at the Medical School eliminated the professor's position, however, and the therapy - promising though it was - was discontinued.
In the absence of any systematic occupational therapy, the patients relieve the tedium of long months of hospitalization in a variety of ways. Some do volunteer work at the hospital, reading to bedfast patients, doing errands, distributing books and supplies. Allowed out during the day after the first few months, they attend movies, concerts, and lectures at the College; some have audited courses. Occasionally - to their embarrassment and his - Salans has encountered a patient sneaking a forbidden sundae at a local icecream emporium.
In the course of the program, "a weight loss of 100 pounds is not uncommon," Salans reports. At first delighted at the prospect of achieving the long-sought goal of slimness, some of the patients become depressed and disconcerted by the time they are discharged. Ironic though it seems, the phenomenon comes as no surprise to Salans: "Other studies confirm that obese people losing weight frequently show signs of depression and hostility. If you've always been obese, you have developed a life-style which protects you. You don't work because you can't get a job; you are insulated from many sorts of competition. It can be very frightening to lose that shield. Some people adjust after they leave the hospital, but a significant number never has to, for the sad reason that most will regain all the weight they have lost."
"It's discouraging," he admits, "but we're dealing with an extremely complex problem, and it spurs me on to learn more and more about obesity so that we'll be able to treat it better."
Much has already been learned through the Dartmouth research: on the clinical level, how the excess adipose tissue alters metabolism, the body's ability to utilize glucose, sugar, hormones and, consequently, how the obese individual tends to become diabetes-prone and insulinresistant; on the basic level, how the enlarged adipose cell burns and stores calories. And Salans and his colleagues - Dr. Samuel Cushman, a bio-chemist investigating the function of adipose cells, and assistants Mary Jane Zarnowski and Ruth Segal - hope to answer more of the essential hows and whys of obesity, with the support of the new five-year grant.
The importance of such basic research can not be over-emphasized, Salans insists. The more spectacular directed research, the crash program to "find a cure" for this ailment or that generally by a certain target date, may capture the headlines - and more easily attract funding - but the painstaking basic laboratory investigation remains the sine qua non on which the dramatic medical "breakthrough" depends.
From what source might a "cure" for obesity emerge? Perhaps, Salans speculates, from the control of the growth of adipose tissue or of the way it synthesizes, stores, and releases calories; behavior, adipose tissue, or appetite centers. "At the moment, however," he emphasizes, "the best form of treatment is prevention, particularly at susceptible ages. And the best therapy thereafter is an intensive long-term program of diet, exercise, and nutritional education."
Despite the seeming munificence of the NIH grants and the funds which the Hitchcock Foundation has provided from its limited resources, the obesity program has been hampered, Salans says, by the enormous per-patient cost - from $15,000 to $18,000 and by the limited professional help through which the patients might receive more lasting benefit from their participation.
" We're making significant progress with a serious public health problem - we think," Salans says. "We know where we are now and where we want to go, but we could do more if we had the funds to bring the best resources of this institution to bear on a disease which will shorten the lives of millions of Americans."
*An opportunity to test this hypothesis has recently arisen through some unrelated work in the treatment of massive obesity going on coincidentally at Mary Hitchcock Hospital. Heretofore, no patient treated for obesity through diet or other conventional therapy has maintained a weight loss for sufficient time to confirm the conclusion clusion that hypercellular obesity is irreversible. But Dr. Rodger Weismann, professor of clinical surgery, has for some ten years been performing a procedure on grossly obese patients, by which a section of intestine is by-passed to reduce the absorption of fat while allowing adequate absorption of protein and carbohydrates. Some of his patients have maintained a weight loss over a long term, and Salans is working with about 100 of them, studying their adipose tissue to determine whether the number of cells does actually decrease after a significant time at reduced weight.
... a fat baby,cute, cuddly,with dimpledcheeks, pudgyarms and legs...
Dr. Salans:Progress with'this too, toosolid flesh ...'
 View Full Issue
View Full Issue
More From This Issue
-
 Feature
FeatureA Delicate Balance
November 1975 By DAN NELSON -
 Feature
FeatureFairly Faced
November 1975 By WILLIAM W. COOK -
 Feature
FeatureSome Faults, Some Solid Achievements
November 1975 By M.B.R. -
 Class Notes
Class Notes1923
November 1975 By WALTER C. DODGE, THEODORE R. MINER -
 Class Notes
Class Notes1942
November 1975 By RICHARD W. LIPPMAN, A. JAMES O'MARA -
 Class Notes
Class Notes1959
November 1975 By DOUGLAS WISE, BARRY R. BLAKE
MARy BISHOP ROSS
-
 Feature
FeaturePoseurs, Impostors, and Scalawags
April 1974 By MARY BISHOP ROSS -
 Feature
Feature"THE KINGDOM OF GOD HAS COME"
October 1974 By MARy BISHOP ROSS -
 Feature
Feature"He could Have talked Satan into abandoning hell"
March 1975 By MARY BISHOP ROSS -
 Article
ArticleRichard Owen Sits on Two Benches: Judicial and Piano
MARCH 1983 By Mary Bishop Ross
Features
-
 Feature
Feature75 Years of Helping Students
APRIL 1971 -
 Cover Story
Cover StoryThey have been called freshies, Pea Greeners, shmen a current phrase that cannot be uttered without sneering.
September 1993 -
 Feature
FeatureSecond Panel Discussion
October 1951 By ARTHUR L. GOODHART -
 Feature
Feature"As I Remember..."
January 1960 By EDWARD CONNERY LATHEM '51 -
 Feature
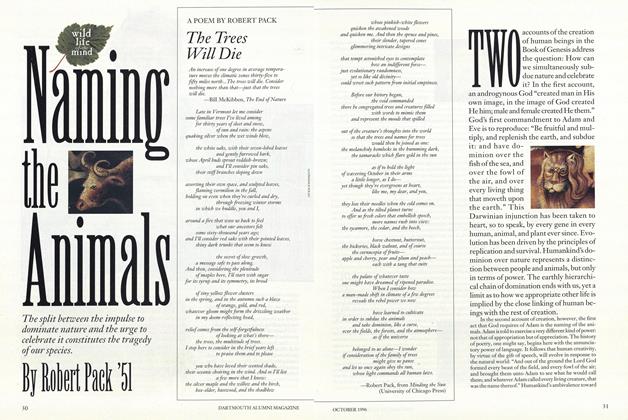
FeatureNaming the Animals
OCTOBER 1996 By Robert Pack '51 -
 Cover Story
Cover StoryHOW TO GET YOUR CONGRESSMAN'S ATTENTION
Sept/Oct 2001 By RUSSELL D. HEMENWAY '49