Imagine showing a rash to your family doctor via a video monitor in your living room. Face to electronic face, you describe your symptoms, she asks you diagnostic questions. She might even have you take your own temperature with a thermometer that plugs right into the computer link-up. Within minutes you have your diagnosis; your pharmacist immediately fills a prescription your doctor ordered by electronic mail. And you never had to leave home, except, perhaps, to pick up your medication. Welcome to a new breed of house calls, part of the burgeoning number of ways that doctors and patients are making connections.
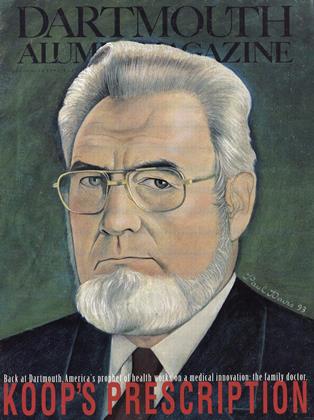
C. Everett Koop "37 has always maintained that house calls are good medicine. Trouble was, of course, that they required busy physicians t travel to their patients, a drawback that made house calls all but disappear. House calls are now coming back, minus the travel time, thanks to a new generation of supercomputers and fiberoptics that bring people together at the touch of a button.
Even when you visit your doctor in person, chances are that your care will increasingly make use of the communications networks that are making the nation—perhaps even the world—seem like one giant clinic. Well-wired doctors at Dartmouth are already experimenting with forwarding images, data, and even live consultations with patients to colleagues across the hospital and across the nation. The Dartmouth doctors have plans to link general practitioners in rural New England to the Dartmouth-Hitchcock Medical Center electronically.
They are not alone. When physicians in Yellowstone National Park have a question about an X-ray, they use a fax-like device to digitize the image and send it over the phone lines to experts at Cody's West Park Hospital, 80 miles away. Baylor College of Medicine in Houston has even bigger plans. According to The New York Times, the school will use a NASA satellite system to enable Texas physicians to consult with surgical patients from Russia to Saudi Arabia.
Perhaps the most audacious tele medical venture is a portable defibrillator manufactured by a New Jersey company that allows doctors to diagnose and treat heart-attack victims over the phone. The product, called MDphone, works like this: If a lay person encounters a heart attack victim and the MDphone is available, he or she simply attaches victim's chest. The MDphone is programmed to dial the closest hospital with doctors trained to use the technology. The attending doctor receives the patient's electrocardiogram over the phone line. If necessary, the physician can push a button to administer a shock and restart the heart. The product has been used hundreds of times and has saved roughly 25 lives, according to a company executive.
Worried that all this techno-care will further displace human care? Not if your doctor has been influenced by a key idea the Koop Institute is trying to bring to national attention: that physicians should take the time to get to know their patients, educate them about treatment options, and listen to their thoughts. Your doctor may augment discussion of treatment plans by giving you an interactive video like those already being produced by Dartmouth's Jack Wennberg (see the May 1991 issue of this magazine). Interactive videos let you explore treatment options at your own pace, arming you with more knowledge than is possible to absorb in a single office visit. Meanwhile, your doctor can consult the latest in "outcomes research" (also a Wennberg initiative) to see which treatment plans actually yield the best results. Then together you can decide what is right for you.
Docs will be linked to the new medical center.
 View Full Issue
View Full Issue
More From This Issue
-
 Cover Story
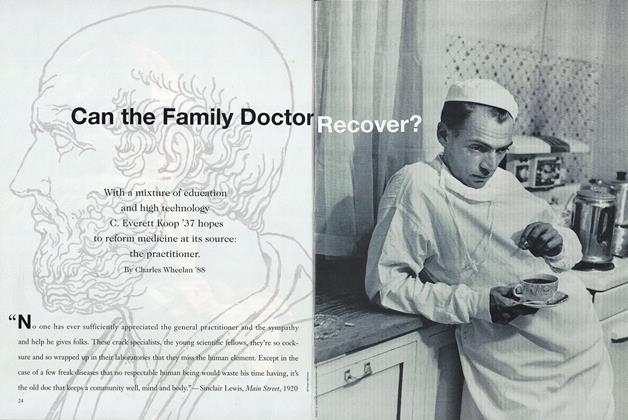
Cover StoryCan the Family Doctor Recover?
November 1993 By Charles Wheelan ’88 -
 Feature
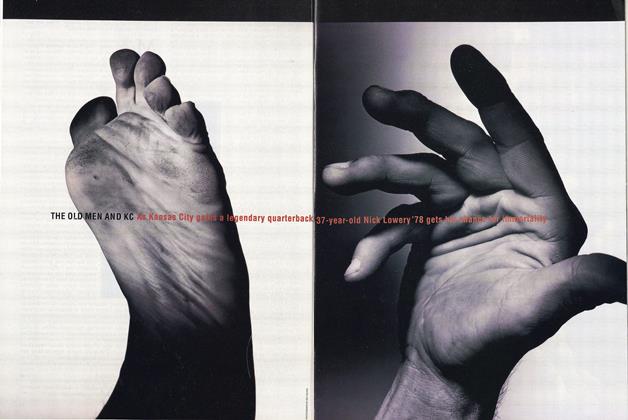
FeatureTHE OLD MEN AND KC
November 1993 By Brooks Clark '78 -
 Feature
FeatureProphet of Limits
November 1993 By Suzanne Spencer '93 -
 Feature
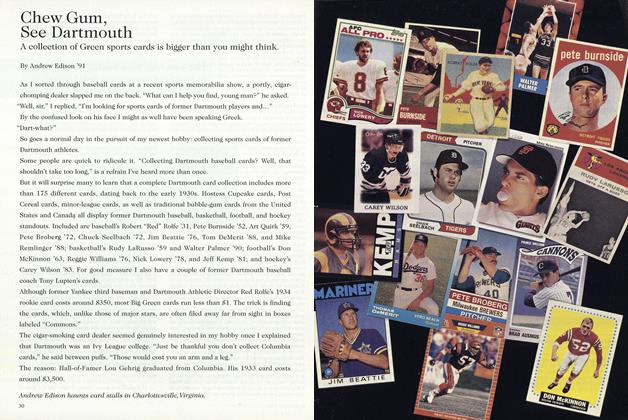
FeatureChew Gum, See Dartmouth
November 1993 By Andrew Edison '91 -
 Article
ArticleDivers Notes & Observations
November 1993 By "E. Wheelock" -
 Class Notes
Class Notes1975
November 1993 By William Blake, W. Blake Winchell
Charles Wheelan ’88
-
 Sports
SportsTurning Pro
June 1987 By Charles Wheelan ’88 -
 Article
ArticleImprover
MARCH 1988 By Charles Wheelan ’88 -
 Cover Story
Cover StoryGREEN INC.
MARCH 1988 By Charles Wheelan ’88 -
 Feature
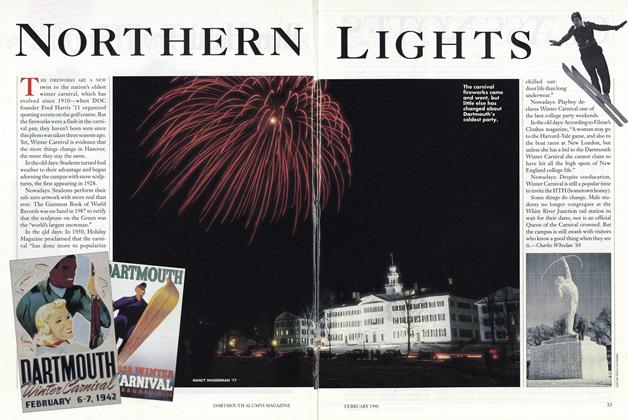
FeatureNorthern Lights
FEBRUARY 1990 By Charles Wheelan ’88 -
 Interview
Interview“A Privileged Position”
Nov/Dec 2003 By Charles Wheelan ’88 -
 Article
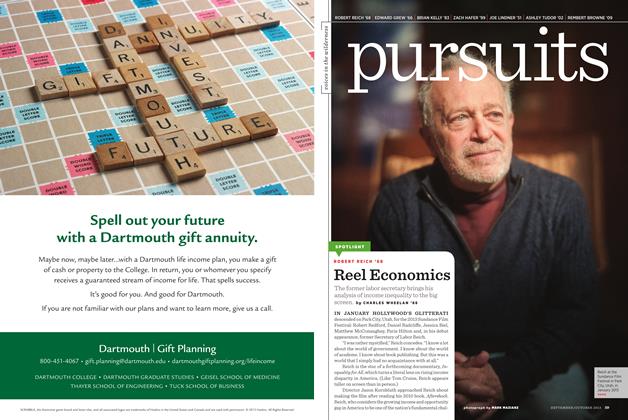
ArticleReel Economics
September | October 2013 By Charles Wheelan ’88