On the brink of breakthrough
Frogs get cancer. So do fish, and people and parrots, dogs, cats, chickens, mice. Even roses. Every kind of living thing is subject to cancer and apparently always has been, for signs of it have been found in the tail bones of a dinosaur.
Cancers, or malignant tumors, result from disorders in the proliferating mechanisms of cells. Normally, cells reproduce in an orderly and self-limiting fashion; when they become cancerous, they multiply abnormally and incessantly. The resulting colony, or tumor, can invade and destroy surrounding normal tissues, and single cancer cells can break off from the mass and metastasize travel through the blood or lymph (the clear fluid that bathes body cells) to set up new colonies in other parts of the body.
Under the microscope, cancer cells look different. The shapes of cancer cells vary and their arrangements are without order. Cancer cells tend to be larger than normal cells and to have greatly enlarged nuclei that often contain more than the usual single nucleolus (small spherical mass). Greater numbers of chromosomes and abnormal chromosomes are often seen in cancer cells. Cancers also resemble embryonic tissues, and fetal protein sometimes reappears in the blood of adult cancer victims. Some normal situations can look like cancers normal repair of injured tissue, for instance, can look quite wild under the microscope, and in the normal pregnancy, cell division proceeds at a rate greater than that of many cancers but the key in the normal situations is self-limitation. Tissue repair and pregnancy reach an end point and conclude. Cancers do not.
Over a hundred forms of cancer are known, and no part of the body is exempt from it. Some cancers grow slowly; others spread like lightning. Most occur with increasing frequency among older people, but some forms occur most often in chil- dren. According to a 1983 publication of the American Cancer Society, 855,000 new cases of cancer will be diagnosed in the United States this year. One of every four people in this country has or will have cancer, and two-thirds of these, 34 million people, will die of it despite surgery, radiation therapy, chemotherapy, and immunotherapy. It is the most difficult nut medical science has ever tried to crack.
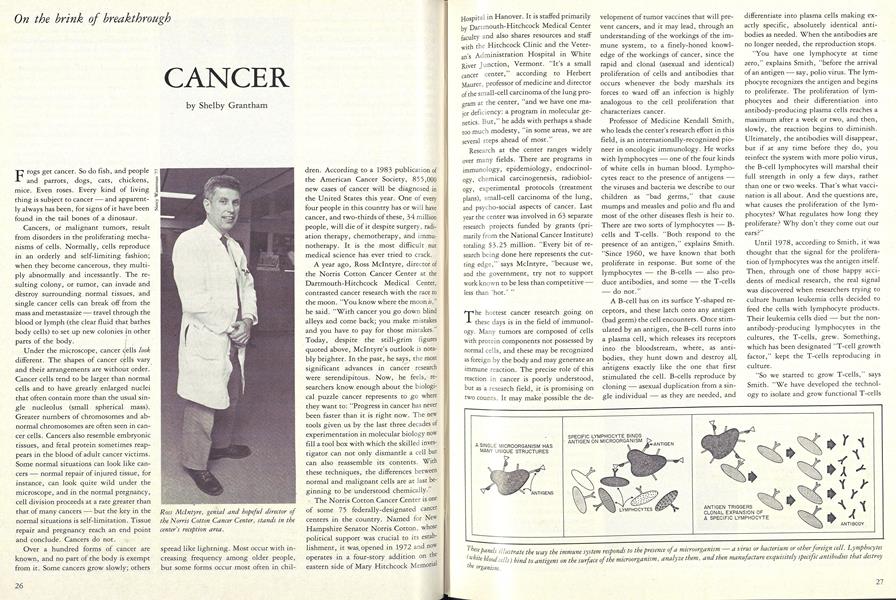
A year ago, Ross Mclntyre, director of the Norris Cotton Cancer Center at the Dartmouth-Hitchcock Medical Center, contrasted cancer research with the race to the moon. "You know where the moonif," he said. "With cancer you go down blind alleys and come back; you make mistakes and you have to pay for those mistakes." Today, despite the still-grim figures quoted above, Mclntyre's outlook is notably brighter. In the past, he says, the most significant advances in cancer research were serendipitous. Now, he feels, researchers know enough about the biological puzzle cancer represents to go where they want to: "Progress in cancer has never been faster than it is right now. The new tools given us by the last three decades of experimentation in molecular biology now fill a tool box with which the skilled investigator can not only dismantle a cell but can also reassemble its contents. With these techniques, the differences between normal and malignant cells are at last beginning to be understood chemically.
- The Norris Cotton Cancer Center is one of some 75 federally-designated cancer centers in the country. Named for New Hampshire Senator Norris Cotton, whose political support was crucial to its establishment, it was. opened in 1972 and now operates in a four-story addition on the eastern side of Mary Hitchcock Memorial hospital in Hanover. It is staffed primarily by Dartmouth-Hitchcock Medical Center faculty and also shares resources and staff with the Hitchcock Clinic and the Veteran's Administration Hospital in White River junction, Vermont. "It's a small cancer center," according to Herbert Maurer, professor of medicine and director of the small-cell carcinoma of the lung program at the center, "and we have one major deficiency: a program in molecular genetics. But," he adds with perhaps a shade too much modesty, "in some areas, we are several steps ahead of most."
Research at the center ranges widely over many fields. There are programs in immunology, epidemiology, endocrinology, chemical carcinogenesis, radiobiology, experimental protocols (treatment plans), small-cell carcinoma of the lung, and psycho-social aspects of cancer. Last year the center was involved in 63 separate research projects funded by grants (primarily from the National Cancer Institute) totaling $3.25 million. "Every bit of research being done here represents the cutting edge," says Mclntyre, "because we, and the government, try not to support work known to be less than competitive less than 'hot.'
The hottest cancer research going on these days is in the field of immunology. Many tumors are composed of cells with protein components not possessed by normal cells, and these may be recognized as foreign by the body and may generate an immune reaction. The precise role of this reaction in cancer is poorly understood, but as a .research field, it is promising on two counts. It may make possible the de- velopment of tumor vaccines that will prevent cancers, and it may lead, through an understanding of the workings of the immune system, to a finely-honed knowledge of the workings of cancer, since the rapid and clonal (asexual and identical) proliferation of cells and antibodies that occurs whenever the body marshals its forces to ward off an infection is highly analogous to the cell proliferation that characterizes cancer.
Professor of Medicine Kendall Smith, who leads the center's research effort in this field, is an internationally-recognized pio- neer in oncologic immunology. He works with lymphocytes one of the four kinds of white cells in human blood. Lympho- cytes react to the presence of antigens the viruses and bacteria we describe to our children as "bad germs," that cause mumps and measles and polio and flu and most of the other diseases flesh is heir to. There are two sorts of lymphocytes B- cells and T-cells. "Both respond to the presence of an antigen," explains Smith. "Since 1960, we have known that both proliferate in response. But some of the lymphocytes the B-cells also pro- duce antibodies, and some the T-cells do not."
A B-cell has on its surface Y-shaped receptors, and these latch onto any antigen (bad germ) the cell encounters. Once stimulated by an antigen, the B-cell turns into a plasma cell, which releases its receptors into the bloodstream, where, as antibodies, they hunt down and destroy all,, antigens exactly like the one that first stimulated the cell. B-cells reproduce by cloning asexual duplication from a single individual as they are needed, and differentiate into plasma cells making exactly specific, absolutely identical antibodies as needed. When the antibodies are no longer needed, the reproduction stops.
"You have one lymphocyte at time zero," explains Smith, "before the arrival of an antigen say, polio virus. The lymphocyte recognizes the antigen and begins to proliferate. The proliferation of lymphocytes and their differentiation into antibody-producing plasma cells reaches a maximum after a week or two, and then, slowly, the reaction begins to diminish. Ultimately, the antibodies will disappear, but if at any time before they do, you reinfect the system with more polio virus, the B-cell lymphocytes will marshal their full strength in only a few days, rather than one or two weeks. That's what vaccination is all about. And the questions are, what causes the proliferation of the lymphocytes? What regulates how long they proliferate? Why don't they come out our ears?"
Until 1978, according to Smith, it was thought that the signal for the proliferation of lymphocytes was the antigen itself. Then, through one of those happy accidents of medical research, the real signal was discovered when researchers trying to culture human leukemia cells decided to feed the cells with lymphocyte products. Their leukemia cells died but the nonantibody-producing lymphocytes in the cultures, the T-cells, grew. Something, which has been designated "T-cell growth factor," kept the T-cells reproducing in culture.
"So we started to grow T-cells," says Smith. "We have developed the technology to isolate and grow functional T-cells continuously in culture. We've known about B-cells for a long time, but this has allowed us for the first time to study the mechanisms responsible for the function of T-cells, as well as how they regulate other cells of the immune system." This basic research Smith and his team are doing has raised a tangle of fascinating questions.
Once it was possible to culture T-cells in quantities large enough to run tests on them, it was discovered that there are two sorts ofT-cell: cytotoxic T-cells and helper T-cells. Cytotoxic T-cells, stimulated by an antigen, develop the ability to put a hole in the membrane of a diseased or invaded cell and destroy it without the mediation of antibodies such as the B-cells produce. "How?" Smith wants to know.
People naturally deficient in cytotoxic T-cells are highly susceptible to the same kinds of infection that people with cancer so often get: viruses and fungal infections that lead to pneumonia, intestinal and mucosal invasion that leads to internal bleeding, even brain bleeding. "Is there a promising connection there?" asks Smith.
The other kind of T-cell, the helper Tcell, makes growth factors B-cell growth factor and T-cell growth factor that promote the proliferation of both Bcells and T-cells. Originally, it was thought that the helper T-cells aided already-proliferating B-cells to mature into plasma cells producing a specific antibody. Now, according to Smith, we know that the proliferation itself depends on the presence of a growth factor as well as on antigen-stimulation. Both are necessary for Bcell proliferation.
"I want to find out the structure of the growth factors," says Smith. "But that's difficult when you can't make enough of them in the laboratory to do tests on. We have had to hover like vultures over splenectomies and tonsillectomies to get lymphocyte populations large enough to allow us to produce it even in low quantities." Just recently, however, one of Smith's graduate students, Steve Gillis, discovered a leukemia whose cells produce 100-fold the usual amount of T-cell growth factor, and, working with that, Smith has learned how to produce T-cell growth factor in quantities large enough to analyze. He has also worked out a method of purifying the growth factor and has discovered that it, like insulin, is a polypeptide hormone. "Now we are working out the chemical structure of purified T-cell growth factor," he explains, "and we are trying to clone the gene responsible for the growth factor."
Another question Smith wants to answer is whether the helper T-cells that make the growth factor for use by other Tcells also make receptors that allow the helper T-cells to receive their own growth factor. Are helper T-cells, when stimulated by an antigen, self-contained proliferation factories? If so, they may be the raw material of some cancers, which batten on the reproducing abilities of the helper Tcells and short-circuit somehow the mechanism that tells them when to stop reproducing.
Smith and his colleagues have, in fact, found one leukemia cell that both makes and receives its own specific growth factor
"We've never before known why leukemia cells grow, and with the discovery of this growth factor, we can begin to study drugs that inhibit the production or action of it, perhaps leading to new, more specific ap- proaches to treatment for leukemia." Smith also wonders whether what happens with this leukemia is what happens with all leukemias. "Or even all cancers," he muses. "Are there growth factors specific to cancers? Different growth factors for different cancers?"
While Smith is pondering such seminal questions in Remsen Hall, Michael Fanger, professor of microbiology, medicine, and biology, is pondering his own set in the medical center's hybridoma laboratory in the basement of the medical school. He too works with cancers of the white blood cells, but his focus is the Bcell, or antibody-producing arm of the immune system. Until 1960, it was believed that only germ cells eggs and sperm were capable of fusing and forming reproducing cells. Then a French scientist discovered that body cells grown in tissue culture could also unite and form hybrids capable of reproduction.
The hybrid cell has the properties of both the parent cells, and in 1975 British researchers put this knowledge to good use and turned the tables on cancer. They reasoned that if they fused a cancer cell, which is virtually immortal, and an antibody-producing plasma cell, they ought to get perpetual production of the specific antibody. The trouble, though, with culturing animal cells is that medical science has not yet found a reliable way to keep a normal cell especially a human cell alive in culture for more than a week. Fortunately, certain strains of mice are, like humans, subject to a form of multiple myeloma (a disease in which cancerous plasma-cell proliferation suppresses all other plasma cell reproduction), and the difficulty was circumvented by fusing a mouse cancer cell with a mouse antibodyproducing cell. The hybrid thus produced could be successfully cultured because it was neither human nor wholly normal.
Thus was born the "hybridoma, " which can be grown in culture forever, forever replicating a specific antibody and allowing the production of large quantities of exquisitely specific antibodies. The advan- tage of these monoclonal antibodies over antibodies produced in the old way, from animals, is that an animal makes hundreds of different antibodies to the single antigen with which it's injected. From this mixture it is difficult to separate out desired single antibodies. The monoclonals, however, produce unlimited quantitites of only one kind of antibody. In theory, these perpetual antibody factories ought to be useful in producing vast laboratory quantities of any specific antibody desired, for use as a serum against virtually any disease.
Scientists such as Fanger are also hopefal that, thus harnessed, cancer can be turned on itself. Before the sixties, it was thought that cancers were too similar to normal tissues to evoke immune responses in their victims. "Now we imagine," says Fanger, "that when a cell becomes malignant, it begins to express new molecules antigens on its surface, which are specific to the malignant cell. It is possible for the immune system to recognize anything and make a specific response to it. There seems to be no limit to the reactions possible in the system it's fascinating. Where there are such things as foreignlooking substances on the surfaces of the tumor cells, there should be an immune response. In fact, there is - it's just not very strong. We don't know why. Perhaps the tumor makes a screen of foreign molecules that protects it against the immune system's antibodies."
At any rate, research is under way to determine how such antibodies could best be used to locate and treat tumors in patients. It-.is thought that putting radioisotopes on the antibodies and sending them out to locate their kind of cancer cell will make it possible to pinpoint the existence of the first smattering of young cancer cells, long before a tumor-ever develops. Such antibodies could also be used not only to find but also to kill tumor cells, or to carry drugs or radiation to them without harming the nearby healthy cells.
Fanger and Professor of Microbiology Edward Bali report that they and their colleagues have, in fact, found several antibodies that react with acute myelogenous leukemia (human bone marrow cancer). so far," he explains, "we have treated three patients with massive doses of these antibodies with limited success. The are not cured, but the number of Cells in their tumors has decreased."
The problem, as Fanger explains, is that the monoclonal antibodies destroy not only the cancerous bone marrow cells, but some normal white cells as well. "So far, says Fanger, "we have not found hybridoma antibodies that react only with the tumor cell."
"Research with different antibodies produced by this method is going on in a number of different places," comments Ross Mclntyre. "Each place hopes that its antibodies will prove effective against cancer. Great advances will be made in this area in the next few years, and we'll be in the thick of it well within my lifetime this work may provide the first practical means of activating the body's own immune system against cancer."
One other approach being used at the Norris Cotton Cancer Center with hybridomas involves giving antibodies indirectly to a patient, by treating with antibodies his or her bone marrow outside the body. Bone marrow transplants of any kind are extremely complicated and have been attempted only since the early seventies at only a few cancer centers in the world. Autologous bone marrow transplantation, the new and still experimental procedure, supercedes older techniques that required locating a marrow donor with immune factors identical to those of the patient a difficult task. The autologous bone marrow transplantation was pioneered at Sidney Farber Institute and involves removing and purging a portion of the marrow of acute leukemia patients whose life expectancy is no more than six months and for whom no other treatment is expected to help.
"We have developed here monoclonal antibodies specific in affinity for myelogenous leukemia and other white cells of the same lineage," says Gibbons Cornwell, professor of medicine and associate director of the center. "Very few other institutions have managed to produce such antibodies." They are going to be put to work soon for a selected leukemia patient, in whose bone marrow are lurking leukemia cells that will, sooner rather than later, bring his or her remission to an ugly end. The patient will be put to sleep and two quarts of bone marrow drawn from the pelvic bone, which is both big and close to the surface. The procedure causes only a little soreness in the hip area, according to Cornwell. The harvested marrow will be taken to the lab and treated with the monoclonal antibodies, so that all leukemic cells are destroyed, but not the stem cells of the marrow itself. The purged marrow will then be frozen at —270° Centigrade to preserve it. After that, the rest of the patient's marrow will be cleaned up.
Using an intensive combination of drugs and irradiation, the doctors will destroy the bone marrow entirely not only all the marrow cells, but also all the regenerating stem cells that could repopulate the marrow. Then the frozen marrow will be thawed and dripped back into the patient's veins. After one month, if all goes well, the stem cells from the reintroduced marrow will have repopulated the patient's marrow with living cells. The difficulty is the one month, during which the patient has no defenses whatsoever against infection and cannot even manufacture red blood cells. For that month, he or she must be isolated, watched like a hawk, and given high doses of antibiotics, platelets, and red blood cells. Cornwell, who heads the center's clinical research program, expects to do the first of these transplants sometime in the next six months. "We are looking for the right patient," he explains, "one aged 16 to 40, in his or her second complete remission of acute myelogenous leukemia, and with cells that react with our panel of antibodies."
Other cancer research described by Cornwell involves blood directly. It has been theorized that metastases are related to clotting, that in order to get a foothold in a distant site, a cancer cell uses a blood clot as a sanctuary in which to start a tumor. The hypothesis is that coagulation sites, where fibrin plugs have formed to stop bleeding, cannot be reached by normal white cells and antibodies that might destroy the cancer cells. The drug nafazatrom, which acts as a potent inhibitor of the platelet aggregation necessary for clotting, is being investigated by cancer center researchers as a possible foil of metastasis. Animals have been injected with cancerous cells that produced metastases throughout their lungs within two weeks, and other investigators have found that nafazatrom administered either before or after the cancer injection results in very few metastases. "This drug may have as its greatest potential the treatment of localized tumors known to recur often even though removed at the primary site," says Corn well. The anticoagulant drug is in phase one trials trials to determine simply whether the drug itself has side effects in humans. So far there have been none, other than some very low level prolongation of normal bleeding time. It is hoped the drug will prove effective in preventing the recurrence of carcinoma of the lung, colon cancer, and malignant melanoma.
The endocrine system of hormone-producing glands is also a focus of research at the center. "Only recently has anyone begun to explore the interface between immunology and endocrinology," explains Associate Professor of Physiology Charles Wira, an endocrinologist. He has a grant to study the way female sex hormones regulate the immune system in women. This tack was suggested by evidence that women on oral contraceptives have suppressed immune systems. They are, for instance, more susceptible to herpes and other viruses and are also at high risk of having a second bout with chicken pox. "Cancer cells grow," explains Wira, "when the immune system fails to recognize them, and we want to understand how the immune system works as a base of information for answering questions about how it fails and allows the growth of a cancer."
Epidemiology the study of the occurrence and spread of disease in a community is contributing to the cause as well. At Norris Cotton, one of the most intriguing projects in this field concerns carrots. Several studies from this country, Japan, and Norway indicate lower incidences of lung, stomach, colon, and prostate cancer some of the biggest killers among people who report eating large amounts of vegetables containing betacarotene, such as carrots, yellow squash,and spinach.
Epidemiologist and internist Robert Greenberg arid dermatologist Steven Spencer are conducting one of the first large scale clinical investigations into the role of vitamin A in cancer prevention. In large quantities, vitamin A itself is toxic to humans; not so beta carotene, a precursor" vitamin A, which the body seems to convert into vitamin A as needed. The study designed by Greenberg is a five-year investigation of the effect of beta-carotene in preventing the recurrence of non-melanoma skin cancer-. This skin cancer, which is relatively innocuous among cancers, is being used as a model for the possible prevention of other cancers. Two thousand skin-cancer patients, who are always at high risk of subsequent skin cancers, will participate in a four-institution study in which neither patients nor physicians know whether carotene or a placebo is being administered. Half the patients will receive 50 milligrams of beta carotene daily (the equivalent of two pounds of carrots), and the entire group will be followed for occurrences of new skin cancers. Professor Greenberg himself is also taking8 the beta carotene "to see what it's like to remember to take a pill every reports that the only anticipated Side effect is a very slight yellowing of the skin.
Another possible link between cancer and diet has emerged from the basic research being done in the laboratories of the center's chemical carcinogenesis program. As so often, research in how not to get cancer begins with research in how to get cancer. In 1970 epidemiologists recognized that the incidence of pancreatic cancer in this country was rising. The pancreas (or "sweetbread") produces many of the body's digestive enzymes, regulates metabolism, and produces insulin. It is a remote, interior organ, and symptoms of pancreatic cancer occur late in the disease, which is seldom successfully treated. Research demanded a way to produce the cancer in the laboratory so it could be studied.
Daniel Longnecker, professor of pathology and director of cancer research training at the center, has had pioneering success in inducing pancreatic cancer in laboratory animals. "In the early seventies," says Longnecker, "we were successful in defining a chemical azaserine that would induce cancer in a specific animal predictably, and we are extending those studies to other chemicals to find out how to produce pancreatic cancer in other species." Once it is known that something produces cancer reliably, the something can be given to a laboratory animal on which various experiments are performed in order to study fac- tors that might influence the known progress of the disease.
One major line of work with the Longnecker animal model is being conducted by Bill Roebuck, professor of toxicology. He puts the azaserine-treated animals on special diets to see whether the diets increase or decrease the pancreatic cancer suffered by the animals. His findings suggest that a diet high in unsaturated fats promotes cancer of the pancreas in these animals, while a diet high in saturated fats appear to have no effect on it. Underfeeding the treated animals and feeding them diets high in proteins, on the other hand, appear to suppress the animals' cancers. Another diet that seems to inhibit the cancers is one high in vitamin A analogs carrots again.
Surgery was the first treatment modern medicine meted out to cancer, and the second major therapy on the scene was ra- diation. The third major cancer treatment chemotherapy is under study at the center in the form of clinical trials. The trials are done in collaboration with several national study groups, since, as Associate Professor of Medicine Herbert Maurer points out, most centers do not see enough of one disease to make treatment research possible. One of the largest clinical trial studies in progress is in small-cell carcinoma of the lung, a program headed by Maurer. Small-cell carcinoma of the lung used to be treated surgically, like other lung cancers. But because of the rampant metastasizing associated with this cancer, surgery was not ideal. Maurer in 1970 designed a combination chemotherapy and radiation protocol (treatment plan) that has proven highly successful in trials all across the country.
Combination therapy radiation plus chemotherapy, or surgery plus radiation, sometimes all three is becoming in- creasingly common as physicians and researchers experiment on willing and otherwise hopeless patients with protocols they think will and often do produce results not possible with one form of treatment alone. One of the most promising new experiments relies on the synergistic effects between heat and radiation. These effects are being tested in several centers across the country, one of which is the Norris Cotton Center.
Hyperthermia, the use of heat to destroy cancer cells, has for the past six years been the focus of a team of researchers drawn from the College's physics department, the Thayer School of Engineering, and the cancer center's radiobiology program, which is headed by Evan Douple, professor of medicine and biomedical engineering. One method of producing hyperthermia utilizes microwave antennae thin, braided gold-wire cables to deliver heat directly into a tumor.
Tumors are thought to be more sensitive to heat than is normal tissue, though researchers are not absolutely certain why. They speculate that heat may make the cancer cell's outer membranes more permeable to chemotherapy drugs and that it may also prevent repair of the damage caused by chemotherapy and radiation. Some cancerous tissue absorbs heat more quickly and easily than normal tissue and seems to retain it longer perhaps because the blood vessels in a tumor are usually tangled and constricted and do not allow heat to escape as quickly as it does through the more open vascular systems of normal tissues. Basically, the more heat delivered to a tumor, the more dead cells, but there is a threshold of thermal pain 45° Centigrade or 113° Fahrenheit beyond which hyperthermia cannot be taken if nerves are involved.
At Norris'Cotton, patients are now being treated with hyperthermia in combination with radiation. Piggybacking on a conventional radiation therapy, Douple coordinates two hour-long sessions of microwave deep-heating with the single radiation session. This radiation treatment, called brachytherapy, involves inserting radioactive "seeds" into the center of a tumor for a certain period, to give a highly localized and slow-release dose of radiation. The patient is put under general anesthesia, and stainless steel hollow needles are inserted through the skin into one end of the tumor and out the other. Hollow nylon tubing is pulled through the needles. The needles are then slipped out and the nylon tubing remains as a channel for the insertion of a link of tiny radioac tive seeds, which is left in place for 72 hours. Before and after the implantation of the seeds, Douple uses the nylon tubing channels as paths for his microwave antennae, which deliver heat at their tips.
"Our preliminary results look promising," says Douple. He feels this method will be especially useful for head and neck and other relatively superficial tumors, and he hopes eventually to find a way to combine hyperthermia with radioactive seeding to treat deep-seated tumors, including brain tumors.
The Norris Cotton Cancer Center is also one of the few centers in the country to have made a definite commitment to research in the psycho-social aspects of cancer. Professor of Psychiatry and Medicine Peter Silverfarb spearheads an effort involving both the promotion of cancer support groups among patients and "hard" science in the behavioral patterns of cancer patients.
There is also a pediatric oncology project making great strides in the treatment both physical and psychological of children stricken with cancer. In both the pediatric oncology program and the support group program, oncologic nurses specializing in cancer have an important role in setting things up so that the patients treated at the Dartmouth-Hitchcock Medical Center and their families have space and time to deal with the many emotions and questions and everyday problems that are part of having cancer and undergoing the grueling treatments often associated with it.
These are some not all of the research projects underway at the Norris Cotton Cancer Center at Dartmouth. Not bad for a "small" center. Funding for research at the center is holding up, despite inflation and federal cutbacks, and the future looks promising. Mclntyre and his colleagues are encouraged about it. Still, Mclntyre says wryly, the most exciting news he could hear about cancer would be that the Reagan administration had announced plans to cancel one Trident submarine and thereby double the amount spent in the country for basic biomedical research. It is an understandable fantasy for a man working in a field on the brink of breakthrough.
Ross Mclntyre, genial and hopeful director ofthe Norris Cotton Cancer Center, stands in thecenter's reception area.
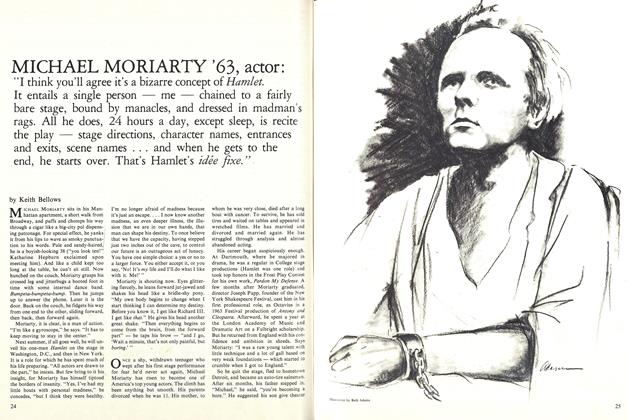
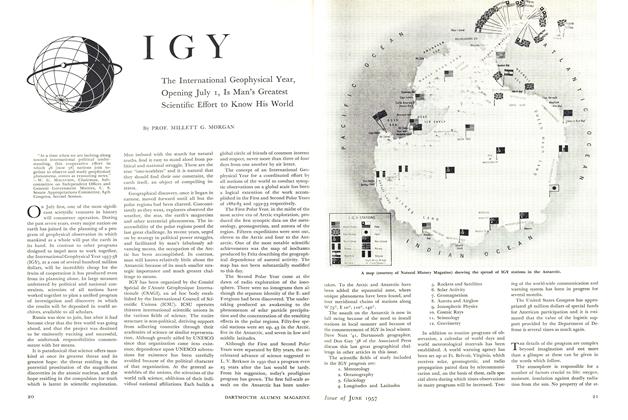
panels illustrate the way the immune system responds to the presence of a microorganism a virus or bacterium or otherforeign cell Lymphocytes(white blood cells) bind to antigens on the surface of the microorganism, analyze them, and then manufacture exquisitely specific antibodies that destroy'the organism.
Immnunologist Kendall Smith waxes eloquentabout B-cells and T-cells.
Fueling his antibody factories, microbiologist Michael Fanger feeds nutrients to hybridoma cells inculture. Inset is a schematic representation of the making of an antibody-producing hybridoma.
The cancer center's associate director. Gibbons Cornwell, hopes soon to find the right patient toreceive the center's first autologous bone marrow transplantation. The diagram on the opposite pageillustrates the procedure.
Pathologist Daniel Longnecker and postdoctoral fellow Barbara Schaeffer discuss the condition ofone of their research animals a white rat in which cancer of the pancreas has been induced by theadministration of azaserine.
Radiobiologist Evan Douple displays the microwave antennae he and his team developed forhyperthermia treatment. Inset above shows an underarm insertion of six stainless steel brachytherapyneedles into a superficial tumor. Nylon inserts have been pulled through the hollow needles prior toremoval of the needles. The nylon tubing will serve as channels to the interior of the tumor, allowingfirst Douple's microwave antennae arid later a link of irradiated "seeds" to be inserted directly intothe tumor to deliver to it both heat and radiation.
Shelby Grantham is assistant editor and staffwriter at the Magazine. In recent months, shehas whritten about Dartmouth's illuminatedmanuscripts and about the College's foreignstudy programs.
 View Full Issue
View Full Issue
More From This Issue
-
 Feature
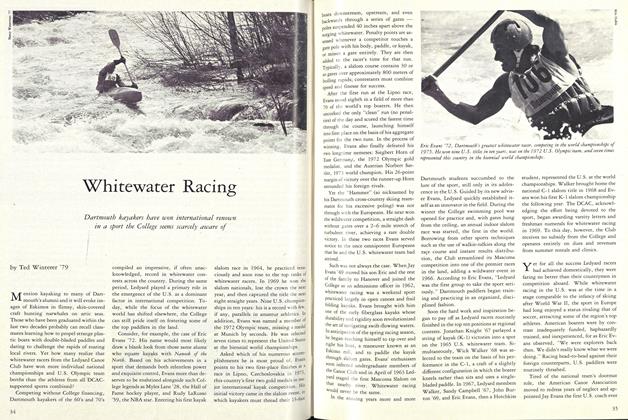
FeatureWhitewater Racing
April 1983 By Ted Winterer '79 -
 Feature
Feature1340 on your radio dial
April 1983 By John May '85 -
 Sports
SportsSports
April 1983 By Brad Hills "65 -
 Article
ArticleThe Arms Race and the Life of the Mind
April 1983 By Stephen J. Nelson -
 Article
ArticleRhodes Scholar
April 1983 By Steve Farnsworth '83 -
 Article
ArticleA Universal Concern
April 1983 By Steve Famsworth '83
Shelby Grantham
-
 Feature
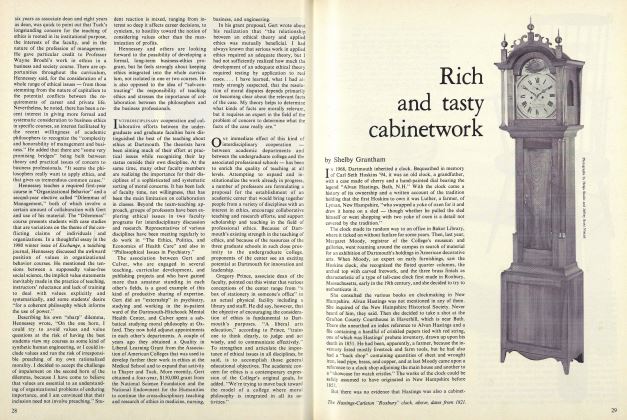
FeatureRich and tasty cabinetwork
March 1981 By Shelby Grantham -
 Feature
FeatureFirst Five Months
DECEMBER 1981 By Shelby Grantham -
 Feature
Feature'One day it came to me: sherry for breakfast was a good idea.'
MARCH 1982 By Shelby Grantham -
 Feature
Feature'Far Out and Daring': Dartmouth Abroad
SEPTEMBER 1982 By Shelby Grantham -
 Feature
FeatureShaping Up
SEPTEMBER 1983 By Shelby Grantham -
 Feature
FeatureIntimate Collaboration
MARCH • 1985 By Shelby Grantham